FOP signs and symptoms
As FOP is rare, many healthcare professionals may not have seen a person living with FOP before in their practice and initial
misdiagnosis
An incorrect diagnosis.
is common.1–3
A diagnosis of FOP can be made based on characteristic clinical signs and symptoms, such as:4
- Turned-in big toes
Recurring flare-ups

 Flare-ups
Flare-ups
Patients with FOP experience sporadic and unpredictable episodes of soft‐tissue swelling, pain, reduced movement, stiffness and warmth, referred to as ‘flare‐ups’.9Extra bone formation (known as
heterotopic ossification

 Heterotopic ossification
Heterotopic ossification
Heterotopic ossification or HO is the presence of bone where bone should normally not exist.5)
However, genetic confirmation is required for a definitive diagnosis.4,5
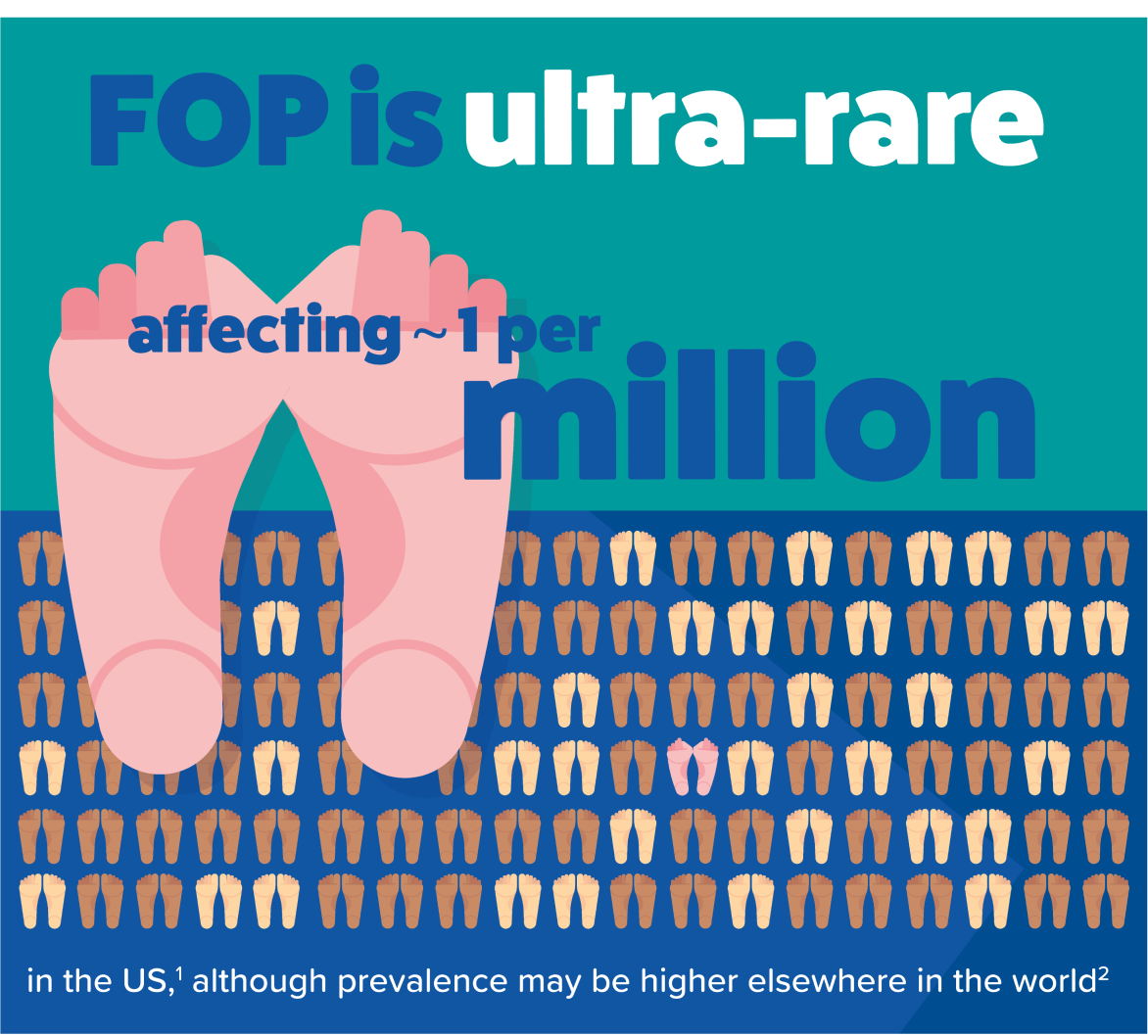
As FOP is rare, many healthcare professionals may not have seen a person living with FOP before in their practice and initial
misdiagnosis
An incorrect diagnosis.
is common.1–3
A diagnosis of FOP can be made based on characteristic clinical signs and symptoms, such as:4
- Turned-in big toes
Recurring flare-ups

 Flare-ups
Flare-ups
Patients with FOP experience sporadic and unpredictable episodes of soft‐tissue swelling, pain, reduced movement, stiffness and warmth, referred to as ‘flare‐ups’.9Extra bone formation (known as
heterotopic ossification

 Heterotopic ossification
Heterotopic ossification
Heterotopic ossification or HO is the presence of bone where bone should normally not exist.5)
However, genetic confirmation is required for a definitive diagnosis.4,5
Short, turned-in big toes

The classic sign of FOP is having shortened and turned-in big toes, which are present from birth. Doctors call it ‘
congenital bilateral great toe malformation![]()
Bilateral - Affecting both sides of the body (e.g., both the left and right big toes).
Great toe - The largest or first toe of the foot. Also commonly known as the ‘big toe’.
Malformation - Irregular or not correctly formed.
’. This makes it look like the big toes are turned inwards towards the other toes, and the joints of the big toes stick out.1,6,7
Nearly all people living with FOP are born with a deformity of both their big toes6,7, and these can be mistaken for
bunions (hallux valgus![]()
Hallux valgus is the medical term for the condition more commonly known as bunions. Bunions occur when there is misalignment of bones at the joint to the big toe, causing it to point inwards towards the other toes.14
).8,9
Swellings, lumps and bumps
Painful soft tissue swellings that occur quickly and without any apparent cause could be another sign of FOP known as a FOP flare-up.4,10 These swellings often start in the upper areas of the body, such as the head, neck and back.4
Soft tissue swellings may be accompanied by redness or a feeling of warmth.10 They may also develop into hard lumps or bumps due to extra bone formation which is characteristic of FOP.6

Other signs and symptoms

Flare-ups may be accompanied by:10
- Pain
- Reduced movement
- Stiffness
- Nonspecific signs of not feeling well, including loss of appetite and lack of energy
Babies with FOP may scoot around on their bottoms rather than crawling due to stiffness of their necks.11–13
Other signs of FOP may include shortened thumbs, other skeletal malformations of the neck area of the spine, hips or legs, and loss of hearing that may be due to extra bone formation in the middle ear.14,15
Correct diagnosis of FOP is important
Getting an early diagnosis of FOP is important as it can make a big difference in how the condition is managed. Once a diagnosis is made, physicians can provide appropriate, guideline-recommended care. This includes avoiding, as much as possible, any interventions, treatments or activities that could worsen the condition.4,5
Any activity or procedure that causes trauma or overstretching of muscles could cause a FOP flare-up and potentially lead to additional bone growth.4

52.5%
Over half of people living with FOP are incorrectly diagnosed before receiving a FOP diagnosis.3,8*
What can happen as a result of being misdiagnosed?9†
67% had surgery that was not needed
68% received medication that they did not need
49% had permanent loss of movement due to a treatment that resulted in new bone formation
Do you think it is FOP?

Do you think it is FOP?
If you think it is FOP, make an appointment with a doctor to discuss your concerns.
Before the appointment, you may find it helpful to note down any signs or symptoms you have noticed or take photographs of the affected area(s) to show the doctor.

Download ‘Let’s talk FOP’ for suggested conversation starters you can use when discussing FOP with the doctor
*Data from the FOP Registry. †Results from a 2001–2002 survey of IFOPA members. 138 members replied, 120 of whom had received an incorrect diagnosis.
1. Pignolo RJ et al. Orphanet J Rare Dis 2021;16:350. 2. Baujat G et al. Orphanet J Rare Dis 2017:12:123. 3. Sherman LA et al. J Bone Miner Res 2020;35:1–337. 4. Kaplan FS et al. Proc Intl Clin Council FOP 2022;1:1–120. 5. Di Rocco M et al. Orphanet J Rare Dis 2017;12:110. 6. Kaplan FS et al. J Bone Joint Surg Am 1993;75-A:220–230. 7. Kaplan FS et al. In: J Bilezikian et al., editors. Primer on the Metabolic Bone Diseases and Disorders of Mineral Metabolism. 9th ed. Washington, DC: American Society for Bone and Mineral Research, 2019:865–70. 8. Sherman LA et al. Poster presentation P-841 at the American Society for Bone and Mineral Research (ASBMR) Annual Meeting, September 11–15, 2020. 9. Kitterman JA et al. Pediatrics 2005;116;e654–61. 10. Pignolo RJ et al. J Bone Miner Res 2016;31:650–65. 11. Pignolo RJ et al. Pediatr Endocrinol Rev 2013;10:437–48.
12. Schaffer AA et al. Spine 2005;30:1379–1385. 13. IFOPA. FOP Symptoms. Available at: https://www.ifopa.org/symptoms. Accessed October 2023. 14. Kaplan FS et al. Hum Mutat 2009;30:379–390. 15. Levy C et al. Am J Audiol 1998;8:29–33. 16. OrthoInfo. Bunions. Available at: www.orthoinfo.aaos.org/en/diseases--conditions/bunions/. Accessed August 2023.