Fibrodysplasia ossificans progressiva (FOP) is a progressive, disabling,
ultra-rare
The Food and Drugs Administration defines a rare disease as any condition affecting less than 200,000 people. There is no formal definition of an ultra-rare disease in the US,29 but in the UK the National Institute for Health and Care Excellence has defined it as a prevalence of <1 per 50,000 people.30
genetic disorder characterized by cumulative and irreversible
heterotopic ossification (HO)
Heterotopic ossification or HO is the presence of bone where bone should normally not exist.3
that leads to loss of mobility and shortened life expectancy.1–3
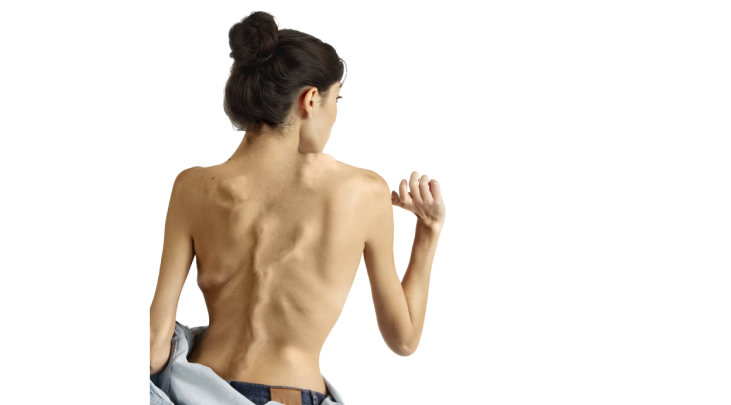
In patients with FOP, anatomically normal bone forms at extraskeletal sites within soft and connective tissues such as skeletal muscles, tendons, ligaments, fascia and aponeuroses.3,4
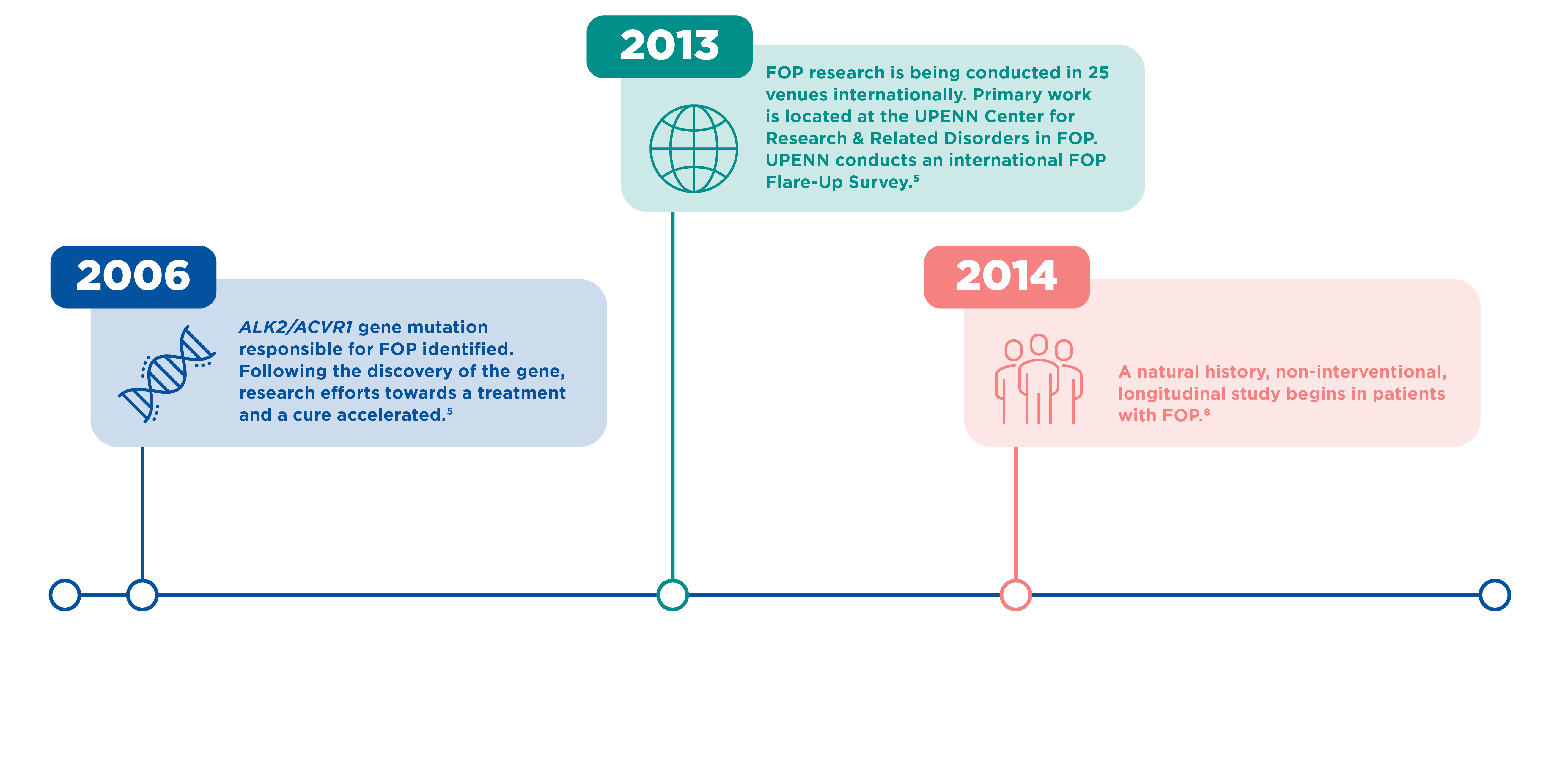
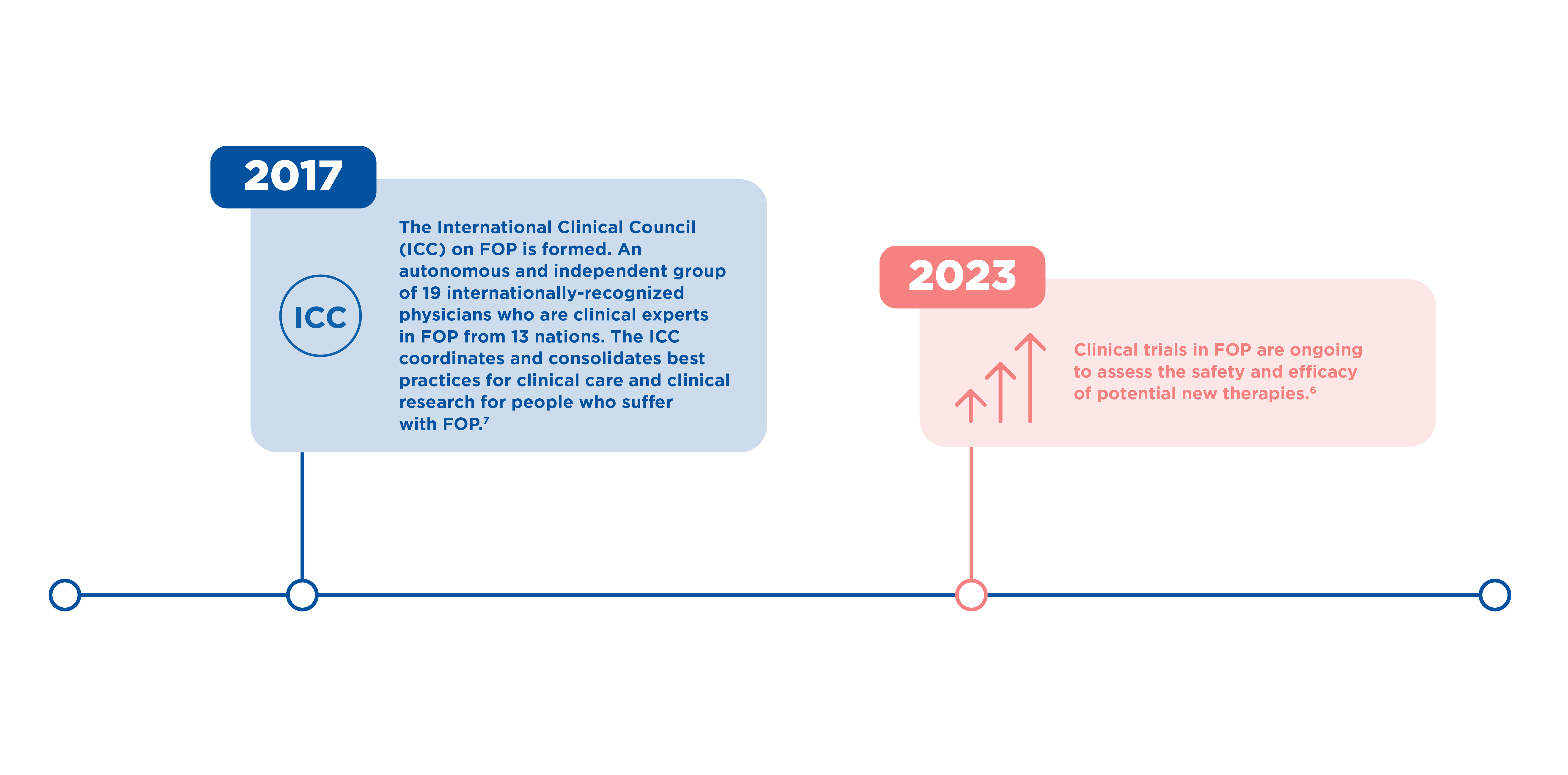
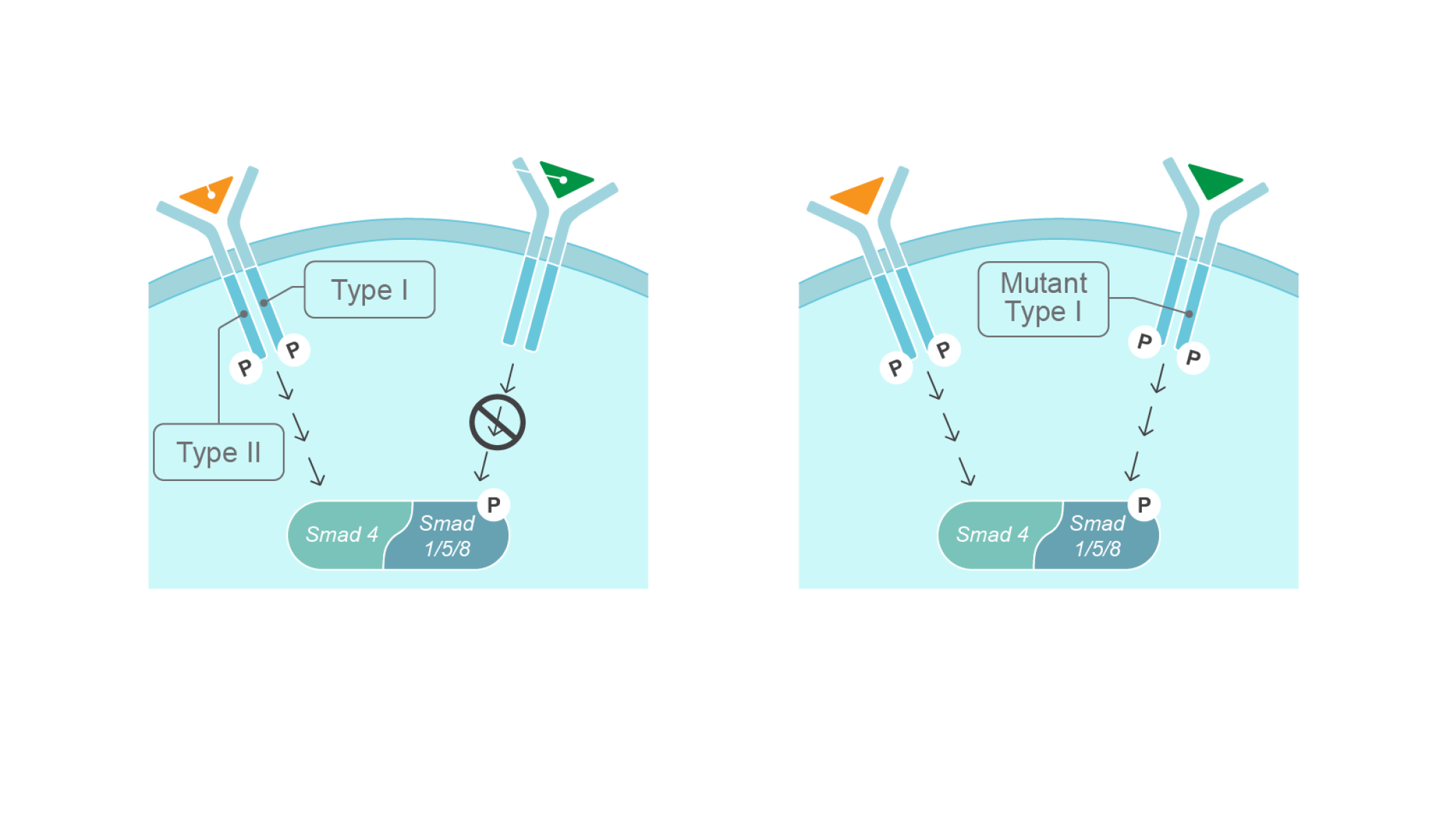
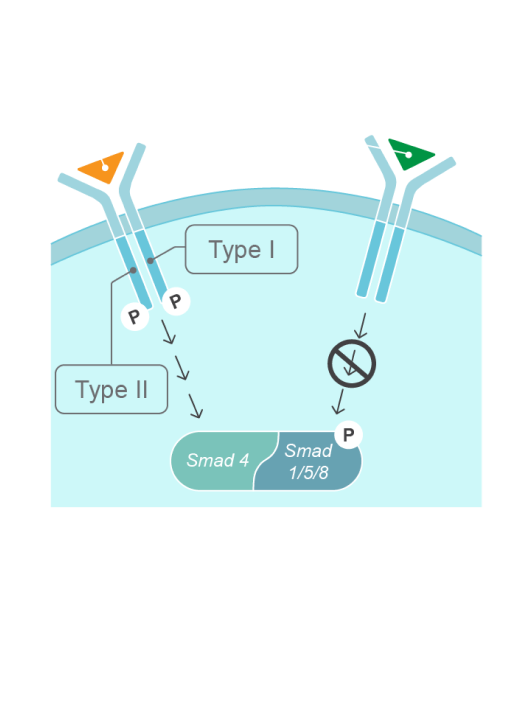
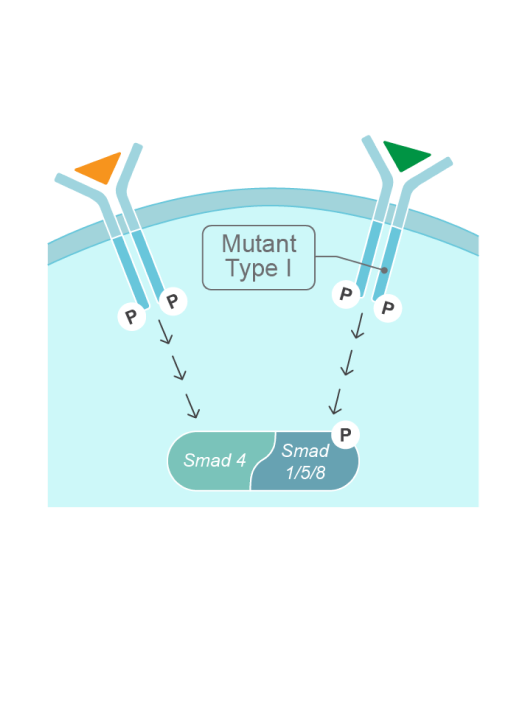
FOP is caused by a mutation in the ALK2/ACVR1 gene, a BMP type 1 receptor.9
Bone morphogenetic proteins (BMPs) are extracellular ligands belonging to the TGF-β superfamily, and play a key role in tissue homeostasis.10–13

Approximately 97% of patients with FOP have the same gain-of-function mutation: R206H in the ALK2/ACVR1 gene4,9,14
Other mutations in the ALK2/ACVR1 gene have been identified in approximately 3% of patients with FOP.14
The mutation is not inherited in most cases of FOP, it arises from a spontaneous missense mutation in the ALK2/ACVR1 gene.9 This mutation changes the ligand response profile of the ACVR1 receptor, so that it becomes activated by the usually antagonistic activin A ligand. This causes increased BMP signaling, leading to abnormal bone formation and in turn, heterotopic ossification (HO).15,16
The R206H gain-of-function mutation in the ALK2/ACVR1 gene causes FOP by changing the response to ligands15,16
The characteristic sign of FOP is congenital bilateral great toe malformation. Almost all patients with FOP are born with this malformation18,19

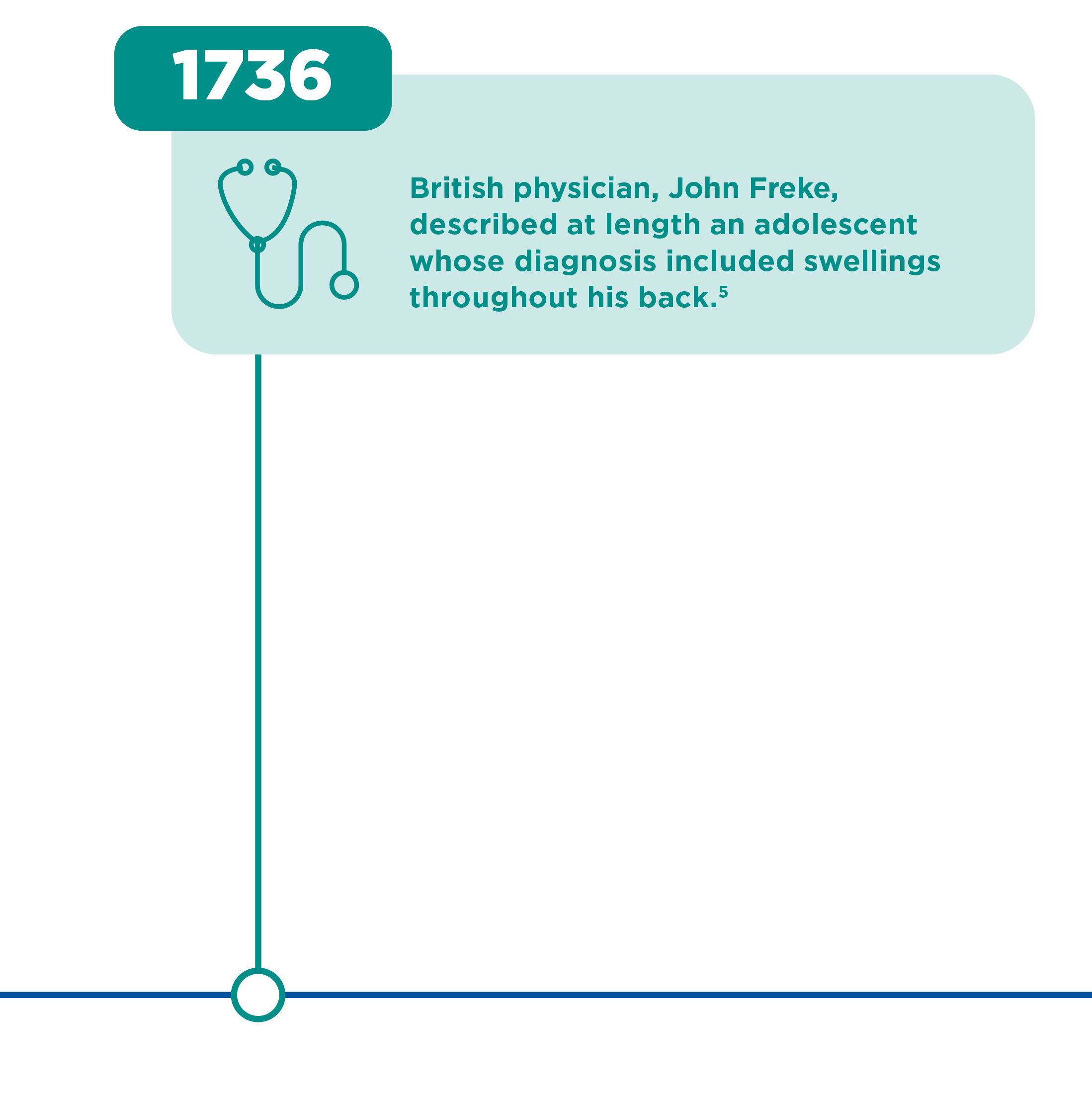
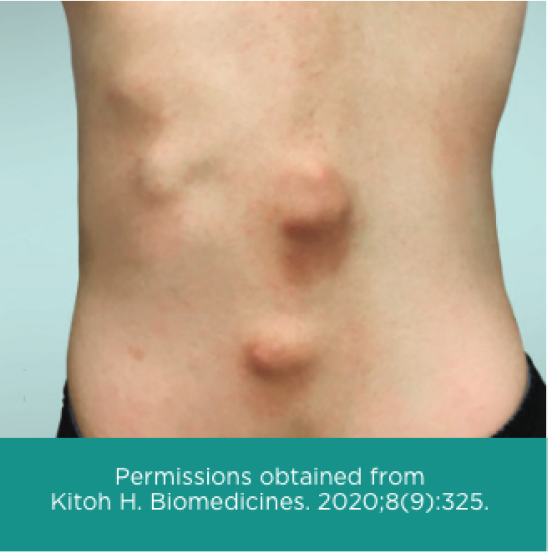
Other signs and symptoms of FOP begin in early childhood and include tumor-like swellings in the head, neck or back17,18

Another sign of FOP in young children is that instead of crawling they will scoot on their buttocks, because of limited neck movement20,21
Patients living with FOP share their stories of what life is like living with this condition
Watch Danie’s Story
Danie describes her experience growing up and living with FOP.
Watch Nadine’s Story
Nadine, patient living with FOP, discusses the symptoms that had the biggest impact on her quality of life.
Flare-ups often present as painful soft-tissue swellings that are warm to the touch19
Patients experience episodes of soft tissue swelling, warmth, pain, stiffness and reduced movement known as flare-ups.19 Flare-ups appear spontaneously or after muscle fatigue, trauma, intramuscular injections or viral infections.22-24 Although some flare-ups regress spontaneously, many lead to heterotopic ossification (HO), which transforms soft and connective tissues, including aponeuroses, fascia, ligaments, tendons and skeletal muscles, into heterotopic bone.3,4
Typically, HO begins in the dorsal, proximal, axial and cranial regions of the body (neck, shoulders, back) and progresses into ventral, caudal and distal regions (trunk and limbs).22–25 HO develops into ribbons, sheets, and plates of extra bone throughout the body and across joints, progressively restricting movement.4,27
Other clinical features observed in patients with FOP are proximal medial tibial osteochondromas, cervical spine malformations, short, broad femoral necks, hearing impairment, and malformations of the thumbs.26

The process of HO begins early in childhood. Some flare-ups occur as a result of viral infection or injury, but others occurs spontaneously.19
1. Pignolo RJ et al. Orphanet J Rare Dis 2019;14:98. 2. Kaplan FS et al. J Bone 2010;92:686–691. 3. Kaplan FS et al. J Bone Joint Surg Am 1993;75:220–230. 4. Pignolo RJ et al. Orphanet J Rare Dis 2011;6:80. 5. History of FOP. International Fibrodysplasia Ossificans Progressiva Association. Available at: www.ifopa.org/history_of_fop. Accessed July 2023. 6. Ongoing Clinical trials. International Fibrodysplasia Ossificans Progressiva Association. Available at: www.ifopa.org/ongoing_clinical_trials_in_fop. Accessed July 2023. 7. The International Clinical Council on FOP. International Fibrodysplasia Ossificans Progressiva Association. Available at: www.ifopa.org/international_clinical_council_on_fop. Accessed July 2023. 8. Pignolo RJ et al. Gen Med 2022;24:2422–2433. 9. Shore EM et al. Nat Genet 2006;38:525–527. 10. Bobacz K et al. Arthritis Rheum 2003;48:2501–2508. 11. Tsuji K et al. Nat Genet 2006;38:1424e1429. 12. Lane KB et al. Nat Genet 2000;26:81–84. 13. Katagiri T and Watabe T. Cold Spring Harb Perspect Biol 2016;8:a021899. 14. Zhang W et al. Bone 2013;57:386–391. 15. Hatsell SJ et al. Sci Transl Med 2015;7:303ra137. 16. Wolken DM et al. Bone 2018;109:210–217. 17. Piram M et al. J Am Acad Dermatol 2011;64:97–101. 18. Kitterman JA et al. Pediatrics 2005;116:e654–e666. 19. Pignolo RJ et al. J Bone Miner Res 2016;31:650–656. 20. Pignolo RJ et al. Pediatr Endocrinol Rev 2013;10 Suppl 2:437–448. 21. IFOPA. FOP symptoms. Available at: www.ifopa.org/symptoms. Accessed July 2023. 22. Connor JM & Evans DAP. J Bone Joint Surg Br 1982;64:76–83. 23. Scarlett RF et al. Clin Orthop Relat Res 2004;423:275–279. 24. Kaplan FS et al. In: Primer on the metabolic bone diseases and disorders of mineral metabolism – Ninth Edition, 2019. J Bilezikian (ed.), Washington, D.C.; The American Society for Bone and Mineral Research: 865–870. 25. Pignolo RJ at al. Clin Rev Bone Miner Metabol 2005;3:195–200. 26. Kaplan FS et al. Hum Mutat 2009;1:379–390. 27. Baujat G et al. Orphanet J Rare Dis 2017;12:123. 28. Kaplan FS et al. J Bone Joint Surg Am 2010;92:686–691. 29. Rare diseases at FDA. U.S. Food & Drug Administration. Available at: www.fda.gov/patients/rare-diseases-fda. Accessed July 2023. 30. Harari S and Humbert M. Eur Res Rev 2020;29:200195.